HYPOXIA REDUCES ABILITY OF SPIKE TO BIND AND REDUCES LEVELS OF ACE2 LEADING TO THE INDUCTION OF CHRONIC MOUNTAIN SICKNESS AND PULMONARY ARTERIAL HYPERTENSION
November 7, 2021
The hypoxia being observed in COVID-19 may be, like so much else with COVID-19, may not be as a direct result of SARS-CoV-2 infection, but the body’s response to the presence of the virus, and in particular, the Spike Protein.
A research article from February, 2021 concluded that hypoxia decreases the attachment of the receptor-binding domain (RBD) and the S1 subunit (S1) of the spike protein of SARS-CoV-2 to epithelial cells. In Vero E6 cells, hypoxia reduces the protein levels of ACE2 and neuropilin-1 (NRP1), which might in part explain the observed reduction of the infection rate. In addition, hypoxia inhibits the binding of the spike to NCI-H460 human lung epithelial cells by decreasing the cell surface levels of heparan sulfate (HS), a known attachment receptor of SARS-CoV-2. This interaction is also reduced by lactoferrin, a glycoprotein that blocks HS moieties on the cell surface. The expression of syndecan-1, an HS-containing proteoglycan expressed in lung, is inhibited by hypoxia on a HIF-1α-dependent manner. Hypoxia or deletion of syndecan-1 results in reduced binding of the RBD to host cells. Our study indicates that hypoxia acts to prevent SARS-CoV-2 infection, suggesting that the hypoxia signalling pathway might offer therapeutic opportunities for the treatment of COVID-19.
Once again, I believe we have been approaching the pathology of COVID-19 completely incorrectly. Hypoxia in COVID-19 IS NOT caused directly by SARS-CoV-2 infection, it is induced by the body in an attempt to mediate the extreme inflammation caused by the Spike Protein’s extreme, traumatic binding. Exposure of primary human bronchial epithelial cells (HBECs) to hypoxia or the prolyl hydroxylase inhibitor dimethyloxaloylglycine (DMOG) resulted in a significantly decreased expression of inflammatory mediators (IL-6, IFN-γ-induced protein 10) in response to ligands for TLRs (flagellin, polyI:C) and Pseudomonas aeruginosa, whereas the expression of inflammatory mediators was not affected by hypoxia or DMOG in the absence of microbial factors.
What is most interesting is that the Spike Protein alone IN HYPOXIC ENVIRONMENTS is able to elicit aberrant signaling, which HbA failed to reverse! It was found that hypoxia downregulated the expression of the ACE2 receptor and increased the critical oxygen homeostatic signaling protein, hypoxia-inducible factor (HIF-1α); however, treatment of the cells with HbA yielded no apparent change in the levels of ACE2 or HIF-1α. Use of quantitative proteomics revealed that S1 spike protein-treated cells have few differentially regulated proteins in hypoxic conditions, consistent with the finding that ACE2 serves as the host viral receptor and is reduced in hypoxia. However, in normoxic conditions, we found perturbed abundance of proteins in signaling pathways related to lysosomes, extracellular matrix receptor interaction, focal adhesion, and pyrimidine metabolism. We conclude that the spike protein alone without the rest of the viral components is sufficient to elicit cell signaling in HPAEC, and that treatment with HbA failed to reverse the vast majority of these spike protein-induced changes.
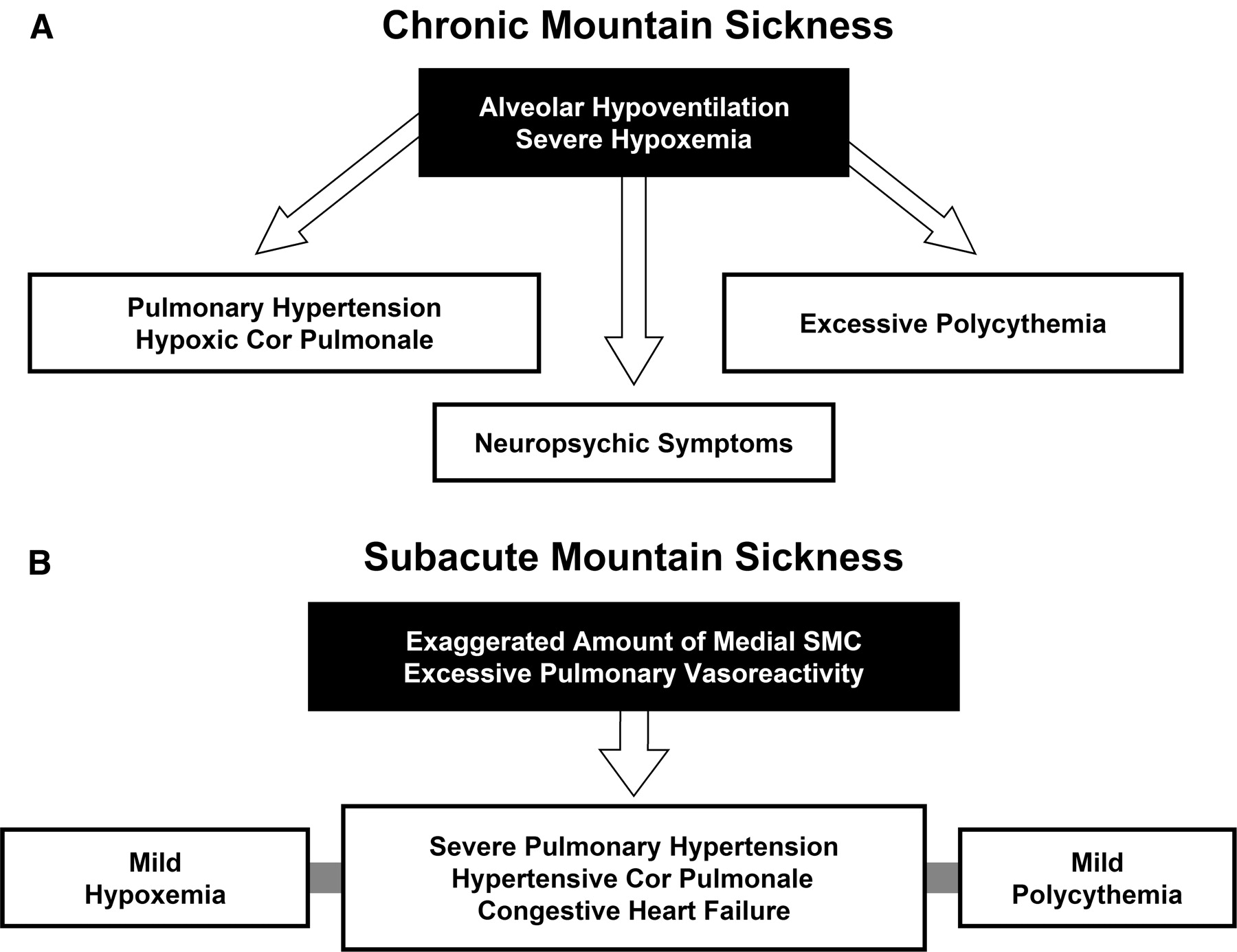
This is why we are observing Altitude Sickness. The body is overcompensating for the hypoxia by creating an excessive number of Red Blood Cells. This explains the Polycythemia which has been observed (and vastly underreported) in COVID-19 patients – including those with mild/asymptomatic cases.
High-altitude polycythemia (HAPC) is a chronic high-altitude disease that can lead to an increase in the production of red blood cells in the people who live in the plateau, a hypoxia environment, for a long time. The most frequent symptoms of HAPC include headache, dizziness, breathlessness, sleep disorders, and dilation of veins.
The end result? What I believe is the compass of COVID-19: Pulmonary Arterial Hypertension. This is the theme of SARS-CoV-2, I believe the Spike Protein will induce fatal Pulmonary Arterial Hypertension. Does the spike remain post infection/exposure? Does it still signal? Do repeated infections/exposures accelerate this process? Is it reversible? Is it inevitably progressive?
These questions must be answered.
Referenced/Related Papers
Associations of high-altitude polycythemia with polymorphisms in PIK3CD and COL4A3 in Tibetan populations
https://humgenomics.biomedcentral.com/articles/10.1186/s40246-018-0169-z
Altitude Induced Pulmonary Hypertension
https://www.ncbi.nlm.nih.gov/books/NBK555925/
Cell-Free Hemoglobin Does Not Attenuate the Effects of SARS-CoV-2 Spike Protein S1 Subunit in Pulmonary Endothelial Cells
https://www.mdpi.com/1422-0067/22/16/9041
Hypoxia and the hypoxia-regulated transcription factor HIF-1α suppress the host defence of airway epithelial cells
https://journals.sagepub.com/doi/full/10.1177/1753425917698032
Hypoxia reduces cell attachment of SARS-CoV-2 spike protein by modulating the expression of ACE2, neuropilin-1, syndecan-1 and cellular heparan sulfate
https://www.tandfonline.com/doi/full/10.1080/22221751.2021.1932607
Chronic Mountain Sickness: Clinical Aspects, Etiology, Management, and Treatment